The science Behind Gondola
A therapy based on solid scientific evidence
Gondola AMPS is not just a technological innovation: it is the result of over 12 years of rigorous scientific research, with 14 published clinical studies and more than 300 patients involved in trials. Every claim about the therapy's benefits is backed by measurable and reproducible evidence.
WATCH THE VIDEO WITH STEFANO TASSIN, GONDOLA'S SCIENTIFIC DIRECTOR
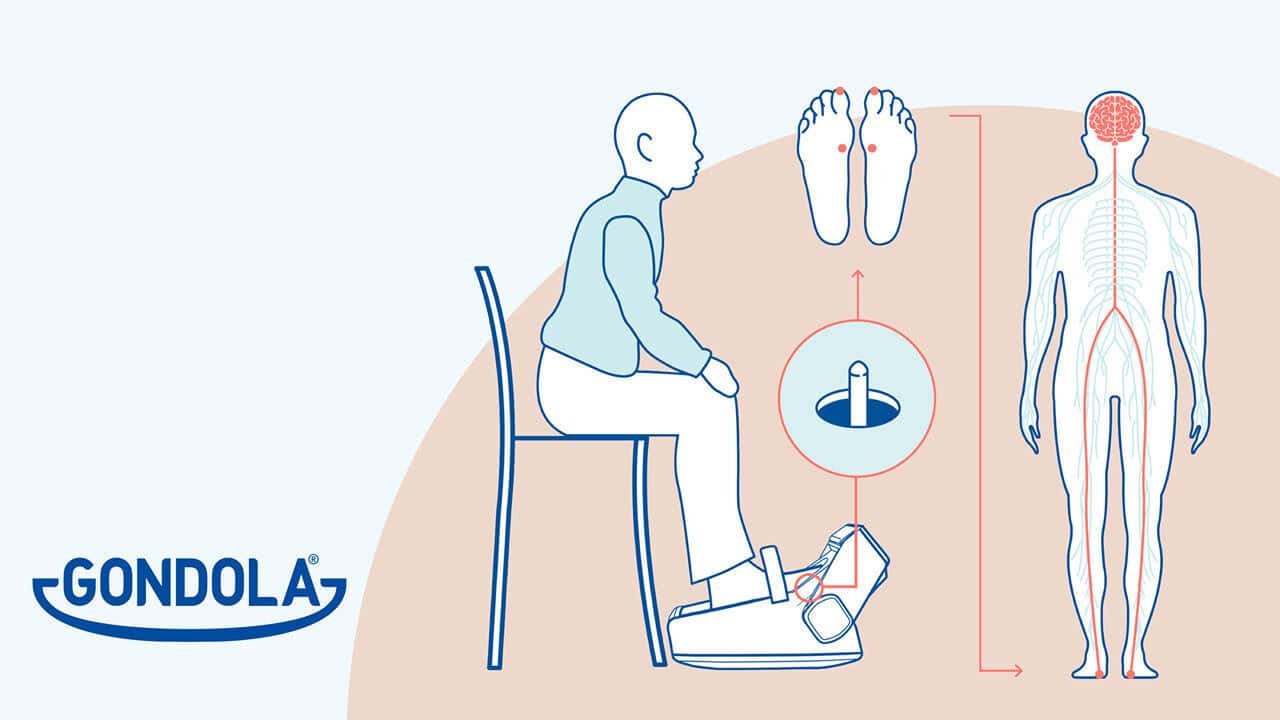
How Gondola AMPS acts on the brain
Studies have shown that after AMPS therapy, BDNF (Brain-Derived Neurotrophic Factor) increases, a protein crucial for neuron health and plasticity. This biomarker indicates that the brain is effectively strengthening its connections.
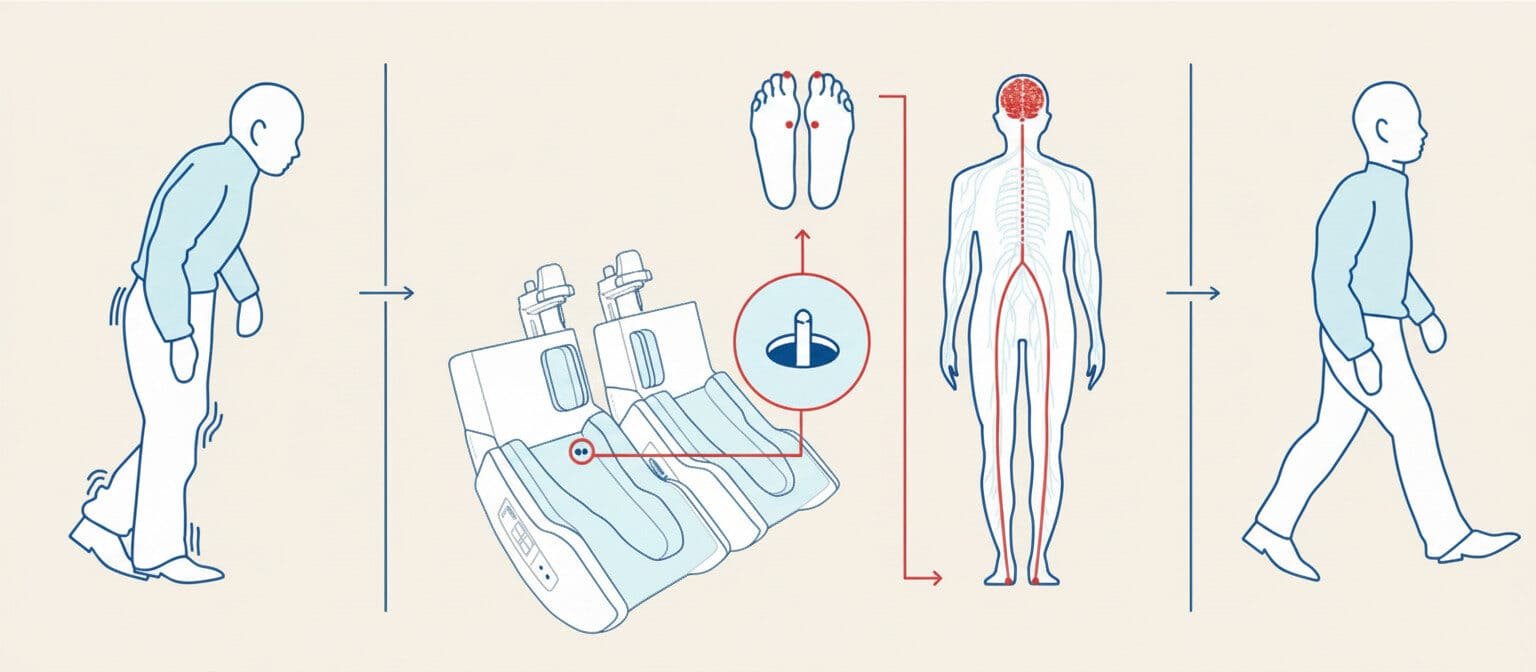
Targeted stimulation
Sensory integration
Synaptic plasticity
Automatism recovered
Research in clinical studies
Do your research and ask questions within the clinical studies concerning Gondola and get immediate answers based on published scientific data.
The 14 published clinical studies
Gondola Medical Technologies is committed to producing impartial scientific evidence on the efficacy of Gondola AMPS therapy. The safety and efficacy of the therapy have been documented in clinical research studies on over 300 patients with Parkinson's disease.
AMPS for the Treatment of Gait Disorders in Parkinson's Disease (2025)
De Pandis et al, Journal of Neuroengineering & Rehabilitation
Advanced-stage multicenter study comparing AMPS with standard therapy for gait disorders in Parkinson's. AMPS proves superior in normalizing rhythm and reducing freezing, with effects persisting for more than a week after the treatment cycle.
Automated Mechanical Peripheral Stimulation for Gait Rehabilitation in Parkinson's Disease: A Comprehensive Review (2023)
Tedeschi R., Clinical Parkinsonism & Related Disorders.
Review of 10 RCTs on AMPS: systematically improves speed, step length, stability, and motor parameters in Parkinson's patients, including those with freezing of gait. The review highlights the utility of AMPS as an add-on therapy but stresses the need for further long-term trials and direct comparison with other rehabilitation strategies.
Plantar Stimulation Alters Brain Connectivity in Idiopathic Parkinson's Disease (2020)
Pagnussat AS et al, Acta Neurologica Scandinavica
Web Link Full Text
In a randomized study of 25 patients with freezing, 8 AMPS sessions increase brain connectivity between the basal ganglia, insula, and sensory areas. Gait velocity improves and correlates with the increase in connectivity; the neuroplastic mechanism is documented via functional MRI.
Mechanical AMPS and Blood Pressure in Parkinson's Disease (2019)
Zamuner AR et al, Journal of Hypertension.
Study highlighting how AMPS improves not only motor parameters but also blood pressure stability in Parkinson's patients with high cardiovascular risk, indicating a potential regulatory effect on the autonomic nervous system.
Peripheral Neurostimulation Breaks the Shuffling Steps Pattern in Parkinsonian Gait: A Double Blind Randomized Longitudinal Study with AMPS (2018)
Galli M et al, Eur J Phys Rehabil Med
AMPS improves spatiotemporal parameters and joint kinematics of gait, particularly breaking the "shuffling" pattern. Effects observed from the first session and progressive up to the sixth.
Automated Mechanical Peripheral Stimulation Effects on Gait Variability in Individuals With Parkinson Disease and Freezing of Gait: A Double-Blind, Randomized Controlled Trial (2018)
Kleiner AFR et al, Archives of Physical Medicine and Rehabilitation.
Web Link Full Text
8 AMPS sessions reduce step variability and asymmetry in patients with freezing, both during simple walking and cognitive dual tasks. The effect is robust and already visible after 4 sessions.
Plantar Stimulation in Parkinsonians: From Biomarkers to Mobility - Randomized Controlled Trial (2018)
Pagnussat AS et al, Restorative Neurology & Neuroscience.
AMPS increases BDNF levels (neuroplastic biomarker), lowers cortisol, and improves walking speed and Timed Up & Go performance compared to the sham group and control subjects.
Automated Mechanical Peripheral Stimulation Improves Gait Parameters in Subjects With Parkinson Disease and Freezing of Gait: A Randomized Clinical Trial (2018)
Pinto C et al, American Journal of Physical Medicine & Rehabilitation.
Web Link Full Text
In the AMPS group, improvements in speed, step length, and hip rotation are observed compared to sham. Effects evident from the first session and consolidated after eight sessions. No relevant adverse events.
AMPS and Postural Control in Subjects With Parkinson's Disease and Freezing of Gait: A Randomized Controlled Trial (2018)
Prusch JS et al, Functional Neurology.
AMPS appears safe and well-tolerated; improvements in postural stability are less evident than those in gait but without adverse events.
Effects of Mechanical Stimulation of the Feet on Gait and Cardiovascular Autonomic Control in Parkinson's Disease (2015)
Barbic F et al, Journal of Applied Physiology.
Pioneering study on the effects of manual plantar stimulation: one treatment on 16 patients improves speed and step length. Suggests the physiological basis of AMPS.
Long-Term Effects of Automated Mechanical Peripheral Stimulation on Gait Patterns of Patients With Parkinson's Disease (2015)
Stocchi F et al, International Journal of Rehabilitation Research.
Web Link Full Text
18 patients underwent 6 AMPS sessions every 4 days: significant and lasting improvement in speed, step, and clinical motor scores. Benefits observed up to 10 days after the cycle.
Acute Modulation of Brain Connectivity in Parkinson Disease After Automatic Mechanical Peripheral Stimulation: A Pilot Study (2015)
Quattrocchi CC et al, PLoS ONE
Web Link Full Text
11 patients, functional MRI pre- and post-AMPS or sham: after a single AMPS session, connectivity increases between sensory-motor areas, striatum, and cerebellum; this does not happen with sham.
The Parkinsonian Gait Spatiotemporal Parameters Quantified by a Single Inertial Sensor Before and After Automated Mechanical Peripheral Stimulation Treatment (2015)
Kleiner AFR et al, Parkinson's Disease.
Web Link Full Text
35 patients: stride length +15%, walking speed +15%, propulsion +30%, with more pronounced benefits in a more compromised subjects.
Timed Up and Go Test and Wearable Inertial Sensor: A New Combining Tool to Assess Change in Subjects With Parkinson's Disease After Automated Mechanical Peripheral Stimulation Treatment (2015)
Galli M et al, International Journal of Engineering and Innovative Technology.
Objective technique with wearable sensors: after AMPS, patients perform the TUG faster, improving acceleration and speed in transitional phases and turns.
Interaction with other treatments
Gondola AMPS complements pharmacological therapies, compensating for the progressive loss of drug efficacy in advanced stages.It also serves as a complementary therapeutic strategy for managing symptoms refractory to DBS, such as freezing of gait, postural instability, and difficulty initiating or modulating steps.
Characteristic
AMPS Gondola
Drugs dopaminergics
Deep brain stimulation
Invasiveness
Non-invasive
Non-invasive
Surgical
Response time
Immediate
30-60 minutes
Continued
Duration effects
2-3 days
3-6 hours
Continued
Side effects
None known
Nausea, dyskinesia
Surgical risks
Gondola Professional
Gondola Professional is a device developed for the use at healthcare Gondola Professional is a device developed for use in healthcare settings to evaluate the effects of AMPS therapy on patients. The device is CE-marked and is reserved for healthcare professionals who have completed the official training provided by Gondola Medical Technologies.
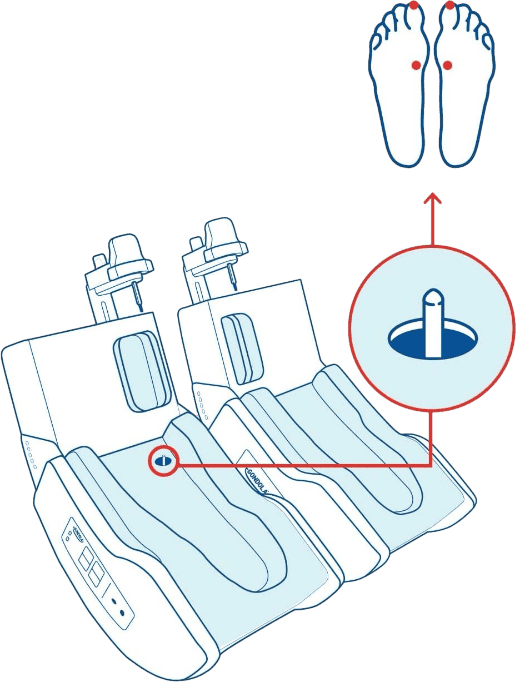
How Gondola Professional works
With Gondola® Professional, delivering AMPS therapy is simple and fast: in just 5 minutes, it is possible to assess the treatment's effectiveness in relation to the patient's condition. Discover how a visit is conducted at one of our centers.